Cholesterol Myths & Facts, Knowing 10 Truths Can Save You
Cholesterol is one topic on which myths and facts are available in plenty … but many people have them all mixed up.
For example, some don’t know the difference between cholesterol and fat and often speak of both interchangeably. Some others may know terms like “good cholesterol” and “bad cholesterol”, but they may not know which type of cholesterol is contained in the foods they consume.
Besides this, there is another important reason we all need to understand cholesterol better. Cholesterol, and other ailments like diabetes, hypertension, or obesity − or a family history of heart disease − can all have a multiplicative effect on our hearts.
Considering that cholesterol is among the most prevalent medical problems, we owe it to ourselves to separate fact from fiction. Here is a list of the 10 most common myths about cholesterol and the facts to know.
Myth 1: All cholesterol – any cholesterol – is bad for you
Fact:
Some types of cholesterol are bad for health while others are essential for good health.
Cholesterol is a fatty substance that is made in the liver. It is found in some foods too. It has value to the body because it helps build cells and make vitamins and other hormones. But, as Heart.org explains, too much of the wrong cholesterol type can pose a problem.
LDL cholesterol (or Low-Density Lipoprotein) is the “bad cholesterol” that can build up on the walls of your blood vessels as plaque and block blood flow. On the other hand, HDL cholesterol (or High-Density Lipoprotein) is the “good cholesterol” that can help flush out the LDL from your bloodstream.
So, your body needs more HDL cholesterol and less LDL cholesterol.
Closely connected to cholesterol are “triglycerides”. They are a type of fat (lipid) found in your blood. If they are not used up as energy by bodily activity, they too start accumulating, hardening your arteries, and adding to your overall cholesterol problems.
Myth 2: I would be able to feel the ailment if I had high cholesterol
Fact:
Unfortunately, unhealthy cholesterol levels show no outward signs or symptoms. You may not even know you have a problem unless it hits such a high level that it manifests as a heart attack or stroke. That’s why doctors insist it is crucial to check your cholesterol levels regularly.
CDC.gov says healthy adults should check their cholesterol every 4 to 6 years. Mayo Clinic recommends cholesterol screenings every 1 to 2 years for people between 45 and 65 years, and yearly tests for those above 65 years.
Myth 3: I cannot do anything to change my cholesterol levels – if it’s there, it’s there
Fact:
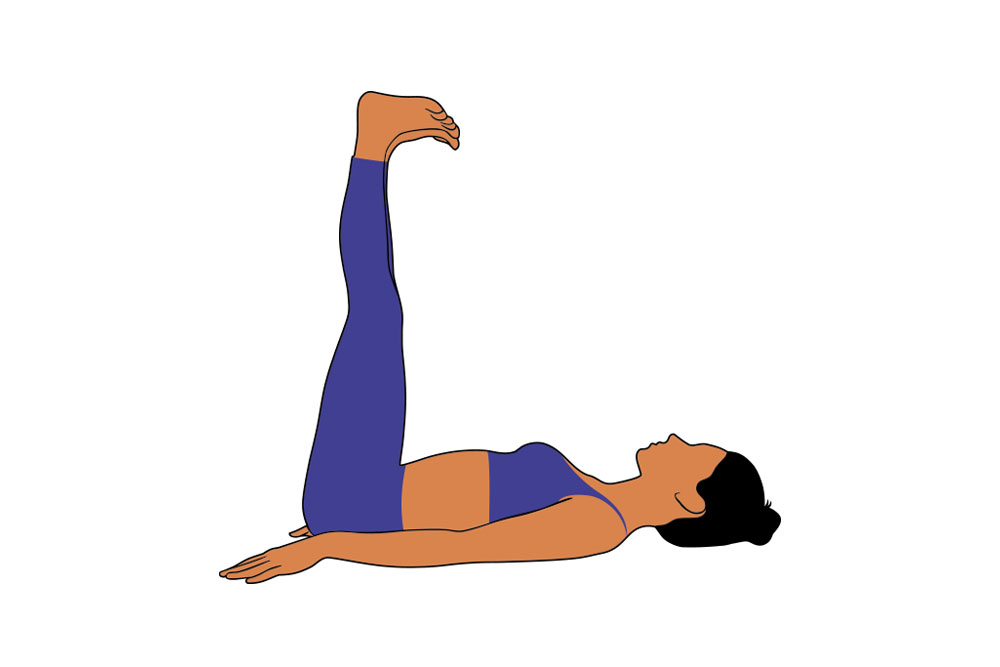
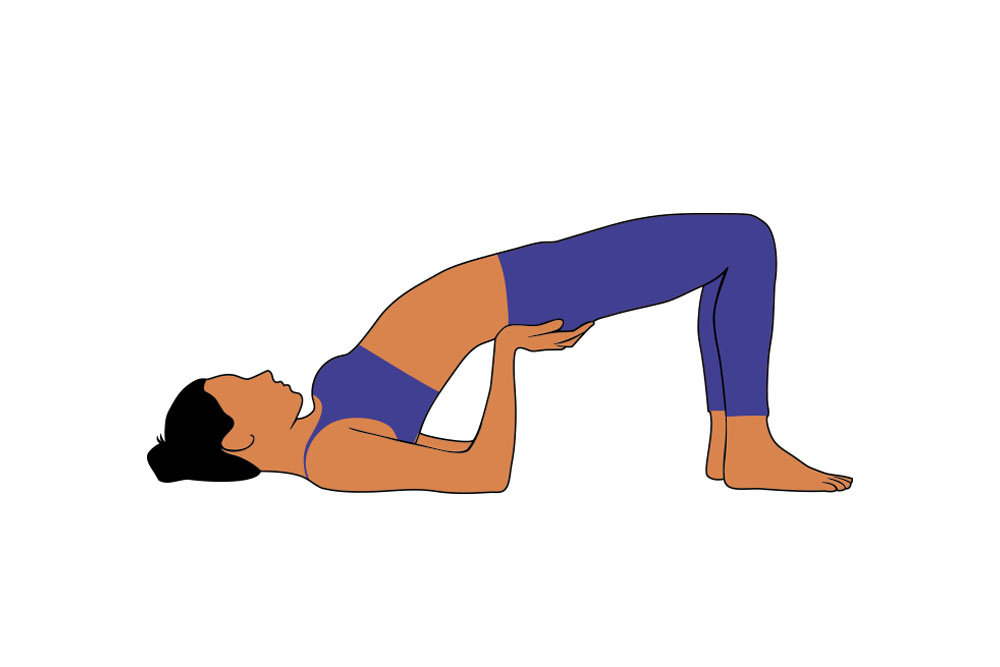
The truth is that you CAN do a lot to help decrease your cholesterol levels. You have to balance your diet, and exercise regularly. You have to stop smoking because it hardens your arteries. Most importantly, you must study your family history of cholesterol-related problems because a large part of cholesterol issues involve genetics.
If you suspect you could have a hereditary tendency towards cholesterol-related ailments, talk to your doctor as early in life as possible. It can help to monitor or keep off the increase of cholesterol as soon as it is detected as a potential problem.
Myth 4: I don’t need statins or other medicines – I can manage my cholesterol with diet and exercise
Fact:
This is one of the most harmful myths to believe. Doctors have a hard time explaining this to patients who think only very high cholesterol levels need medical interventions. On the contrary, as soon as doctors say so, cholesterol patients must start taking “statins” (a group of medicines that can help lower the LDL cholesterol in the blood).
Other cholesterol control forms – like diet and exercise – can be in addition to medication. But they cannot take the place of prescribed statins. Please take in this message with extreme seriousness. Talk to your doctor and if he asks you to start taking statins, waste no time and get going.
Myth 5: Eating foods with a lot of cholesterol will not make my cholesterol levels go up
Fact:
This myth goes wrong in two ways. Firstly, you cannot buy and eat cholesterol from a store. Cholesterol is often hidden in some form of fats in other food products your buy and consume. So you may not know if you are eating a lot of cholesterol or not.
Secondly, if your dietician says certain foods are high in LDL cholesterol (like foods made with trans-fats), it’s better to reduce eating them. If there are other foods rich in HDL cholesterol (like some nuts or Omega-3 fatty acids), your dietician may recommend eating more of them. But either way, don’t overdo anything. Moderation, even with a good diet, is the key.
In general, wholesome home-cooked food is always better than ready-processed bought food or eating out. You know what is going into the food as ingredients, and you can control the balance of every meal with a good assortment of whole grains, pulses, fresh vegetables, nutritious fruits, essential nuts, healthful condiments, and cholesterol-lowering fats and oils.

Myth 6: I am a healthy weight, so it cannot be that I have high cholesterol
Fact:
This myth suggests people’s typical inability to differentiate between fat (obesity) and cholesterol. As we said before, cholesterol does not manifest outwardly as body weight, flab, or body fat.
Cholesterol becomes an issue for those people whose bodies cannot process cholesterol efficiently. For example, a person can be born with a genetic inability to process cholesterol optimally. That person may have a normal body weight and trim appearance on the outside … but inside the body, the cholesterol processing systems may perform sub-optimally. Regular tests are essential to locate and treat cholesterol imbalances.
Myth 7: Children don’t need to worry about cholesterol
Fact:
Children can have high cholesterol levels, just like adults. This is especially true for those children who may have inherited high cholesterol levels from one or both parents. Such children can be prone to premature heart attacks or strokes.
Further, all parents must always be careful of what their children eat or what ailments their bodies may silently carry. An increasing number of hereditary disorders go unnoticed in children, only to blow up when they are young adults.
Talking to your children about active exercise, and making home food enjoyable are ways to teach good lifestyle habits. Children alone cannot exacerbate their latent cholesterol problems unless parents give in to their demands for unhealthy goodies. Parents should beware of acting as enablers.

Myth 8: I take my prescribed statins regularly, so I can eat whatever I want
Fact:
Isn’t this the way we all kid ourselves? We think just because we are on good medications, we can thereafter leave the medicines to work, and we can go about our old happy-go-lucky lifestyles even after being diagnosed with a serious disease. Unfortunately, you can’t just hope the statins prescribed for your cholesterol need no other corrective actions from you.
As any good doctor will tell you, the job of the statins is to lower the bad LDL cholesterol in your system, but they can’t help you much if you pile in more and more of the LDL via unhealthy food. You can help the statins work effectively if you act responsibly and control your intake of bad cholesterol foods. According to the Cleveland Clinic, exercise reduces triglycerides, raises HDL, and has a slight lowering effect on LDL too. So exercise also helps statins work better.
Myth 9: I’m under 40 and a woman, so I don’t need to have my cholesterol checked
Fact:
It’s a pervasive myth that only men get cholesterol-related ailments more than women, especially if they are around 40 years or older. That belief doesn’t seem to be validated by research.
Dr. Robert Greenfield, a board-certified cardiologist, lipidologist, and internist at Memorial Care Heart & Vascular Institute, California, says that women − especially after menopause − lose the protective effects of estrogens. He quotes a CDC research showing that in people of the 40-59 age group, the prevalence of high total cholesterol was 10.5% in men and 12.1% in women.
He believes that women of that age group begin to accelerate their risk of heart disease and develop the same risks as men. He sums it up neatly when he says, “Heart disease is an equal opportunity employer.”
Myth 10: If the nutrition label shows no cholesterol, the food is heart-healthy
Fact:
Food labels are notorious for the nutrition information they hide behind jargon. There are consumer complaints galore on the Net, and especially on social media, on how people fell for food labels of certain processed foods that said cholesterol levels were low while they were not.
A lot of this angst may also be because people cannot understand what they read on food labels. Usually, labels list a breakdown of fats like this: Total Fat, Saturated Fat, Trans Fat, Polyunsaturated Fat, Monounsaturated Fat, and Cholesterol. If you read just the cholesterol content of the food and it looks low, you may mislead yourself.
MyDoc.com says saturated and trans fats should be as low as possible, even at zero. They raise your total and LDL cholesterol. Polyunsaturated and monounsaturated fats are better for you and can be eaten in moderation. Read the ingredients list further down the label … if you see words like “margarine”, “shortening”, “hydrogenated”, or “partially hydrogenated”, steer clear of the food. These clog your arteries.
In summary …
One of the smartest ways to tackle your cholesterol problems is to be able to correct your beliefs. After that, you’ll find that good knowledge steers you in the right direction towards improving your health.
Cholesterol, as we said, has a direct bearing on your heart. Treat your cholesterol early and with good care − and you’ll treat your heart responsibly too.