Facts About Weight – And Why You Shouldn’t Believe Myths
The most important fact about weight is that overweight people get a bad rap, often erroneously. They are assumed to be lazy, or averse to exercise. They are believed to be overeaters, without self-discipline − or doomed by fat genes. They are also seen as people who are out of touch with reality, and ignorant that excess weight can cause serious diseases. This is needless and harmful stereotyping.
Overweight people usually suffer a lot because they may be genuinely trying to lose weight but they don’t realize it can be a tug of war. They lose some weight, and soon their bodies fight them to add the weight back. Why is this so?
Many people soon discover this “metabolic rate” dilemma when trying to lose weight. Metabolic rate refers to the rate at which your body burns the food and fat it consumes to create energy. To lower weight, you do exercises or eat certain foods to raise your metabolic rate.
But when you lose weight, the body’s metabolism slows down. So, in a way, your weight loss success becomes the cause for slowing down any further weight loss. The weight and fat then begin to reappear. And the cycle goes on and on. People often call it the “yo-yo weight loss effect”.
How do you escape this “yo-yo cycle”? Read on …
3 facts about weight and its relationship to metabolic rate
There are 3 interesting facts about how your metabolic rate can be increased – and you can thereby hope to reach your ideal body weight without the “yo-yo effect” …
Your Basal Metabolic Rate (BMR) is quite important for weight problems
Healthline states, “Basal metabolic rate is the number of calories your body needs to accomplish its most basic (basal) life-sustaining functions.”
Why is BMR key to body weight? Because it shows how active or inactive your everyday daily life is. The more generally active you are, the more calories you burn without additional exercise. Therefore, you must aim for an active movement-oriented life to lose weight.
Having more muscle raises your metabolic rate and weight loss
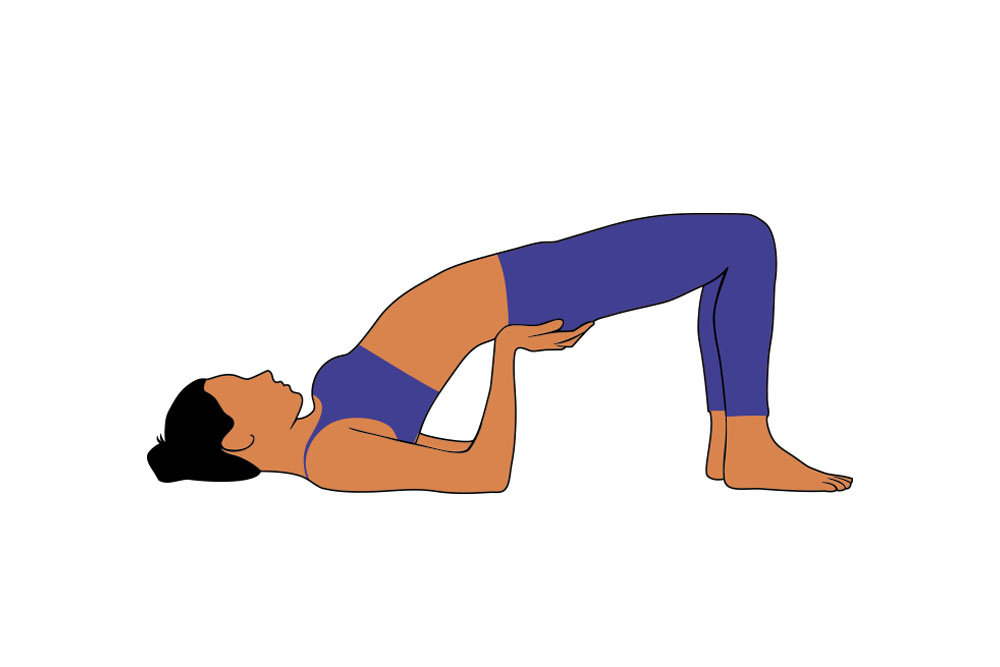
Physical fitness coaches always include muscle-building and weight training during exercise routines. The more muscle you have, the more calories your burn. In your body, your legs have the most muscle area … so the more you exercise using your legs, the more calories you can burn.
Mayo Clinic advises that if your body weight is composed more of fat than muscle, you must consciously build up your muscles in addition to just burning calories by movement.
Eating protein-rich food boosts your metabolism and aids weight loss

You burn calories even to digest food. Of all the food types – carbohydrates, fats, and proteins – it’s the proteins that burn the most calories during digestion.
According to a paper published by the National Library of Medicine, US, increasing protein intake boosts metabolism by roughly 15 to 30 percent. So, all in all, eat more proteins to lose weight.
Myths about weight − and the facts to replace them
There are a number of us who have wrong ideas about weight loss. The first step to losing weight is to lose these erroneous beliefs.
Myth 1: “If I exercise a lot, I can eat almost anything because I am burning it all.”
The fact:
To lose weight, you need to burn more calories than you consume. You can’t do that, though, unless you count calories and keep track of your intake and output. Medical News Today has a table that shows a “healthy calorie deficit” between intake and output of calories, calculated by age and gender.
What should your calorie deficit be? WebMD states, “A good rule of thumb for healthy weight loss is a deficit of about 500 calories per day. That should put you on course to lose about 1 pound (approximately 0.45 kgs) per week. This is based on a starting point of at least 1,200 to 1,500 calories a day for women and 1,500 to 1,800 calories a day for men.”
Myth 2: “Drinking a lot of water can increase my body weight. I should take diuretics.”
The fact:
Water can increase metabolic rate and burn more calories. This is contrary to how people think they can reduce their weight by taking diuretics. What are diuretics? They are medications that rid the body of water (usually prescribed for some other illnesses by doctors). Often, they are misused by those who want to lose weight. But this kind of water-weight loss is not the same as healthy weight loss due to reduced body fat or body mass.

A novel finding in a study published by Oxford Academic says, “Drinking 500 ml of water increases metabolic rate by 30% in both men and women. The increase in metabolic rate was observed within 10 minutes after completion and reached a maximum of 30–40 minutes after water drinking. The effect was sustained for more than an hour.” Hydration seems to help in weight control.
Myth 3: “Body weight is a genetic handover. Whatever you try, you cannot fight your genes.”
The fact:
Research does indeed show that your genes can lead to weight issues. But, here’s the fact. You are not fated to be fat just because your parents are; you can fight genetics with proper diet and exercise. There’s one gene that’s now getting a lot of attention, called FTO. WebMD claims scientists found that people with this gene have a 20% to 30% higher chance of obesity. If a cause has been found, the cure may hopefully not be far behind.
Besides genetics, your environment, lifestyle, and healthy choices may also significantly affect how much you weigh. One interesting theory is that obesity may run in families both because of genetics and the family habits inculcated around diet and exercise. What your parents teach you about healthful habits may be as crucial as the hereditary tendencies they pass on to you.
Assessing your risk for weight-related diseases
Ailments like cholesterol, diabetes, hypertension, obesity − or a family history of heart disease − can all have a multiplicative effect on our hearts. If you are overweight or obese, you will only compound your health and heart risks if you have any of these ailments. Plus, beware of the silent stress symptoms below:
- You smoke a lot or drink too much alcohol without self-control
- You have a lonely, sedentary lifestyle, often digitally-addicted
- You feel silently worried about most things, including your weight
- Your work and relationships don’t gel with your personality type
The wise saying goes, “When you have a weight problem, don’t just ask what you are eating. Ask what is eating you.”
The 6 unbeatable weight loss best practices
Just do these 6 things every day without fail, and your weight will drop away naturally over time …
- Eat healthfully, keeping track of calories – and get the right calories into your body (i.e., more lean proteins).
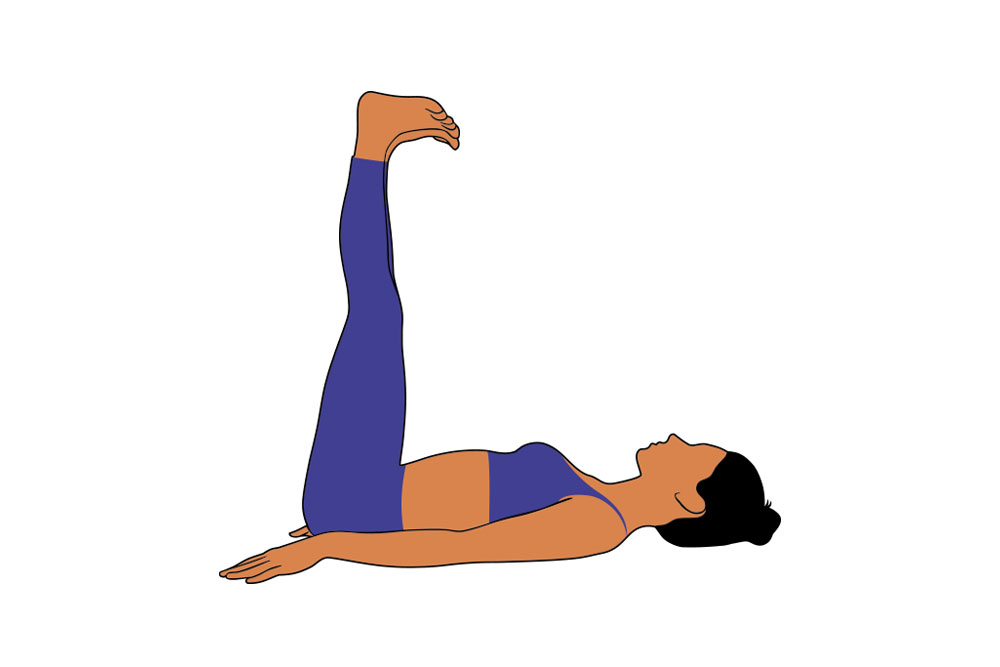
- Exercise for at least 30 minutes daily with muscle building routines for the legs. Don’t focus only on upper body muscles.
- Stay stress-free. Learn yoga, meditation, breathing exercises, and mindful living. Don’t fret about being fat. It’s solvable.
- Keep your body well hydrated. Drink lots of water (as plain water) – not as water in tea or coffee or juices or fizzy drinks.
- Check your health for other illnesses like hypertension, diabetes, cholesterol, and heart disease. Tell the doctor about your genetics.
- If you have genetic ailments, teach your children early on how to eat and exercise healthfully to stave off any premature diseases.
In summary …
There is a deep connection between body weight and metabolic rate. Often, they work at cross-purposes and defeat your good intentions to reduce weight. But despite this, it’s imperative to follow a proper diet and exercise to lose weight and reduce the risks of many weight-related ailments. All these ailments eventually lead to heart disease.
Blow away the myths in your mind about weight, and learn the facts. Assess the risks of your weight and stress on your health and heart. Most of all, be conscious and responsible about your weight issues. By doing so, you will treat your heart responsibly.